Mega Doctor News
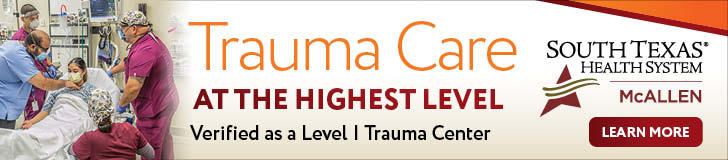
Zika – 1952
Zika virus disease is caused by the Zika virus, which is spread to people primarily through the bite of an infected mosquito (Aedes aegypti and Aedes albopictus). Zika virus was first discovered in 1947 and is named after the Zika Forest in Uganda. In 1952, the first human cases of Zika were detected and since then, outbreaks of Zika have been reported in tropical Africa, Southeast Asia, and the Pacific Islands. Zika outbreaks have probably occurred in many locations. Before 2007, at least 14 cases of Zika had been documented. Because the symptoms of Zika are similar to those of many other diseases, many cases may not have been recognized. In March 2015, Brazil reported a large outbreak of rash illness, soon identified as Zika virus infection, and in July 2015, found to be associated with Guillain-Barré syndrome. In October 2015, Brazil reported an association between Zika virus infection and microcephaly. Outbreaks and evidence of transmission soon appeared throughout the Americas, Africa, and other regions of the world. To date, a total of 86 countries and territories have reported evidence of mosquito-transmitted Zika infection.
The majority of people infected with Zika virus do not develop symptoms. Symptoms are generally mild including fever, rash, conjunctivitis, muscle and joint pain, malaise, and headache, and usually last for 2–7 days. There is no treatment available for Zika virus infection or its associated diseases.
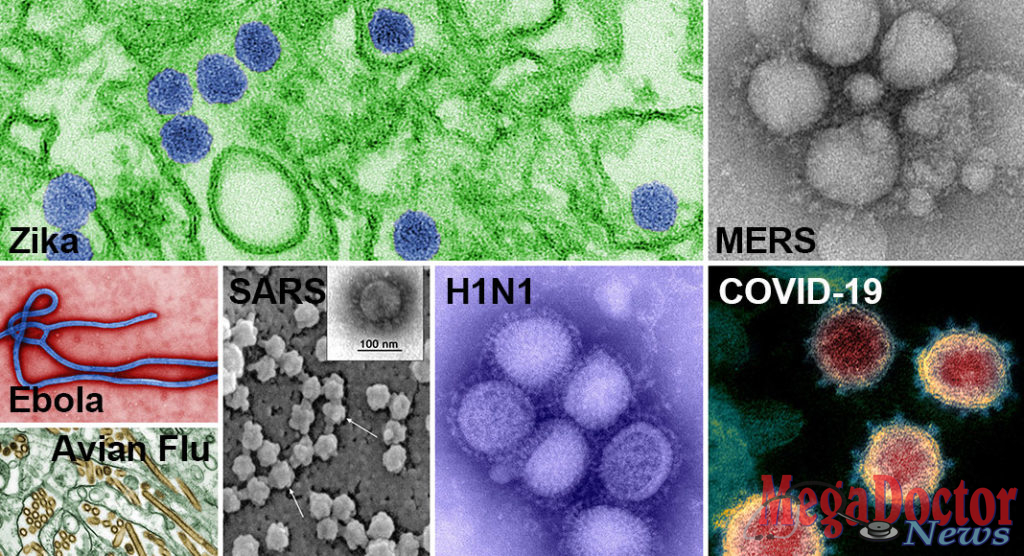
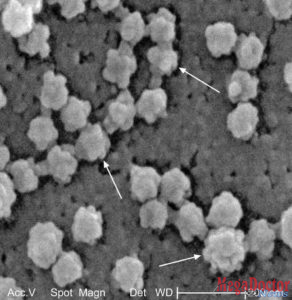
EBOLA – 1976
Ebola Virus Disease (EVD) is a rare and deadly disease in people and nonhuman primates. The viruses that cause EVD are located mainly in sub-Saharan Africa. People can get EVD through direct contact with an infected animal (bat or nonhuman primate) or a sick or dead person infected with the Ebola virus.
Since its discovery in 1976, the majority of cases and outbreaks of Ebola Virus Disease have occurred in Africa. The 2014-2016 Ebola outbreak in West Africa began in a rural setting of southeastern Guinea, spread to urban areas and across borders within weeks, and became a global epidemic within months; 11 people were treated for EVD in the U.S., two of whom died. The majority were infected with the Ebola virus outside of the U.S. and either medically evacuated into the U.S. for treatment or entered the country as a regular airline passenger. In addition, two nurses who cared for a sick Ebola patient contracted EVD, marking the first known transmission of EVD in the United States.
Since the current outbreak of Ebola emerged in August 2018, nearly 400 CDC volunteers have deployed to the Democratic Republic of Congo (DRC), neighboring countries, and Geneva to help fight the disease.
The FDA has approved the Ebola vaccine rVSV-ZEBOV (tradename “Ervebo”) for the prevention of EVD. The rVSV-ZEBOV vaccine has been found to be safe and protective against only the Zaire ebolavirus species of ebolavirus.
Avian influenza – 1996
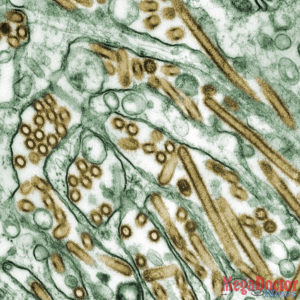
Not all avian influenza viruses cause disease in humans. However, some can infect humans and cause severe disease. The most well-known of these are avian influenza H5N1 viruses that circulate in poultry around the world and in North America. Outbreaks caused by avian influenza viruses occur In U.S. domestic poultry from time to time.
These outbreaks were caused by North American lineage viruses (North American lineage avian influenza viruses have very rarely infected people) that are different from Asian H5N1 (first detected in 1996 in geese in China) and Asian H7N9 (first reported in China in March 2013) viruses that have caused human infections resulting in serious illness and death in other parts of the world. Asian H5N1 and Asian H7N9 viruses have not been detected in people or birds in the United States. More than 700 human infections with Asian HPAI H5N1 viruses have been reported to WHO from primarily 15 countries in Asia, Africa, the Pacific, Europe, and the Near East since November 2003. On July 25, 2008, the Food and Agriculture Organization (FAO) released an Avian Influenza Disease Emergency Situation Update, reporting that H5N1 pathogenicity was continuing to gradually rise in endemic areas but the avian influenza disease situation in farmed birds was being held in check by vaccination.
The first report of human infection with Asian H5N1 in the Americas was in Canada on January 8, 2014, and occurred in a traveler recently returning from China. Although human infections with this virus are rare, approximately 60% of the cases have died.
Evidence suggests that some antiviral drugs can reduce the duration of viral replication and improve prospects of survival, however ongoing clinical studies are needed.
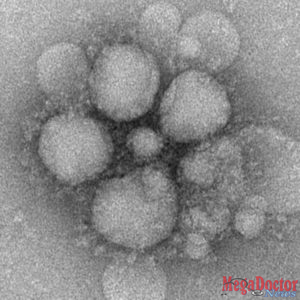
SARS (Severe Acute Respiratory Syndrome) – 2002
Severe acute respiratory syndrome (SARS) is a viral respiratory illness caused by a coronavirus, called SARS-associated coronavirus (SARS-CoV). SARS appeared in November 2002 in the Guangdong province of southern China and was first reported in Asia in February 2003. Over the next few months, the illness spread to more than two dozen countries in North America, South America, Europe, and Asia before the SARS global outbreak of 2003 was contained. According to the World Health Organization (WHO), a total of 8,098 people worldwide became sick with SARS during the 2003 outbreak. Of these, 774 died. In the United States, only eight people had laboratory evidence of SARS-CoV infection. All of these people had traveled to other parts of the world where SARS was spreading. SARS did not spread more widely in the community in the United States. The implementation of appropriate infection control practices brought the global outbreak to an end. Experimental vaccines are under development.
Swine Flu – 2009
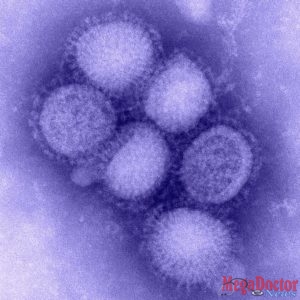
The Pandemic H1N1/09 virus is a swine-origin Influenza A virus subtype H1N1 virus strain that was responsible for the 2009 flu pandemic. This strain is often called swine flu by public media.
It was detected first in the United States and spread quickly across the United States and the world. This new H1N1 virus contained a unique combination of influenza genes not previously identified in animals or people. This virus was designated as influenza A (H1N1)pdm09 virus.
The (H1N1) pdm09 virus was very different from H1N1 viruses that were circulating at the time of the pandemic. Few young people had any existing immunity (as detected by antibody response) to the (H1N1) pdm09 virus, but nearly one-third of people over 60 years old had antibodies against this virus, likely from exposure to an older H1N1 virus earlier in their lives. Since the (H1N1) pdm09 virus was very different from circulating H1N1 viruses, vaccination with seasonal flu vaccines offered little cross-protection against (H1N1) pdm09 virus infection. While a monovalent (H1N1) pdm09 vaccine was produced, it was not available in large quantities until late November—after the peak of illness during the second wave had come and gone in the United States. From April 12, 2009 to April 10, 2010, CDC estimated there were 60.8 million cases (range: 43.3-89.3 million), 274,304 hospitalizations (range: 195,086-402,719), and 12,469 deaths (range: 8868-18,306) in the United States due to the (H1N1) pdm09 virus.
On August 10, 2010, the WHO declared an end to the global 2009 H1N1 influenza pandemic. However, (H1N1) pdm09 virus continues to circulate as a seasonal flu virus and causes illness, hospitalization, and deaths worldwide every year.
MERS – 2012
Middle East Respiratory Syndrome (MERS) is a viral respiratory illness that is new to humans. It was first reported in Saudi Arabia in 2012 and has since spread to several other countries, including the United States. Most people infected with MERS-CoV developed severe respiratory illness, including fever, cough, and shortness of breath. About 3 or 4 out of every 10 patients reported with MERS have died.
At the end of November 2019, a total of 2,494 laboratory-confirmed cases of MERS, including 858 associated deaths (case–fatality rate: 34.4%) were reported globally; the majority of these cases were reported from Saudi Arabia (2,102 cases, including 780 related deaths with a case–fatality rate of 37.1%).
MERS represents a very low risk to the general public in the U.S. Only two patients in the U.S. have ever tested positive for MERS-CoV infection—both in May 2014—while more than 1,300 have tested negative. There is no specific antiviral treatment recommended for MERS-CoV infection. Individuals with MERS often receive medical care to help relieve symptoms. For severe cases, current treatment includes care to support vital organ functions.
COVID-19 – 2019
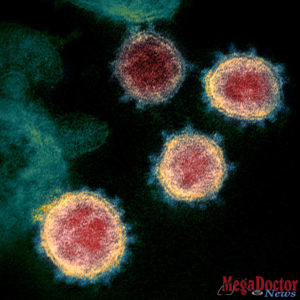
COVID-19 is an infectious disease caused by the most recently discovered coronavirus. This new virus and disease were unknown before the outbreak began in Wuhan, China, in December 2019 and has now been detected in more than 150 locations internationally, including in the United States. The virus has been named “SARS-CoV-2” and the disease it causes has been named “coronavirus disease 2019” (abbreviated “COVID-19”).
On January 30, 2020, the International Health Regulations Emergency Committee of the World Health Organization (WHO) declared the outbreak a “public health emergency of international concern” (PHEIC).
On January 31, Health and Human Services Secretary Alex M. Azar II declared a public health emergency (PHE) for the United States to aid the nation’s healthcare community in responding to COVID-19.
On March 11, WHO publicly characterized COVID-19 as a pandemic.
On March 13, Donald Trump, the President of the United States declared the COVID-19 outbreak a national emergency.
Global efforts at this time are focused concurrently on lessening the spread and impact of this virus. The federal government is working closely with state, local, tribal, and territorial partners, as well as public health partners, to respond to this public health threat.
Content source: CDC and WHO