
Mega Doctor News
CDC, the Mexican Ministry of Health, and U.S. state and local health departments are responding to a multinational outbreak of fungal meningitis among patients who had procedures under epidural anesthesia in Matamoros, Tamaulipas, Mexico. Officials have identified two clinics associated with the outbreak: River Side Surgical Center and Clinica K-3. These clinics were closed on May 13, 2023. Anyone who had procedures under epidural anesthesia in these clinics from January 1 to May 13, 2023, is potentially exposed and at risk for fungal meningitis. Learn what to do if you are at risk.
As part of the collaboration between the United States and Mexico, the Mexican Ministry of Health provided CDC a list of U.S. residents who had procedures at River Side Surgical Center or Clinica K-3 from January 1 to May 13, 2023. CDC and state and local health departments are working to reach all people with potential exposures and advise them to go to their nearest emergency room for diagnostic testing for fungal meningitis. Testing includes magnetic resonance imagining (MRI) of the brain and a lumbar puncture (LP), also called a spinal tap.
Additional people with potential exposure who were missing from the original list are being found and contacted through public health investigation, outreach efforts, social media, and by family and friends as they learn about the outbreak.
Information for People with Potential Exposure
If you had epidural anesthesia in Matamoros, Mexico, at River Side Surgical Center or Clinica K-3 from January 1 to May 13, 2023:
- Go to the nearest emergency room as soon as possible to be evaluated for fungal meningitis, even if you do not currently have symptoms.
- Some affected people tested positive for infection when they had mild or no symptoms. Receiving treatment early can prevent severe illness.
- Fungal meningitis can start off mild and very quickly become a life-threatening illness.
- Consider printing and sharing this web page to help make sure staff and healthcare providers are aware of the situation and recommended tests.
- If you cannot go to an emergency room (for example, because it is too far away), consider calling your local health center or urgent care facility to see if they can do MRIs and spinal taps. In most situations, the emergency room will be the best or only option.
- When you arrive, tell emergency room staff that you need to be evaluated for possible fungal meningitis. Tell them that you recently had epidural anesthesia at one of the clinics in Mexico involved in this outbreak.
Important Points
If you had epidural anesthesia in Matamoros, Mexico, at River Side Surgical Center or Clinica K-3 from January 1 to May 13, 2023, you should go to the nearest emergency room as soon as possible to be evaluated for fungal meningitis, even if you do not currently have symptoms.
Starting treatment right away if you are found to have fungal meningitis greatly increases the likelihood of survival.
Fungal meningitis infections are not contagious and are not spread from person to person.
Cancel any elective procedure that involves an epidural injection of an anesthetic in Matamoros, Mexico—and any travel associated with such a procedure—until there is evidence that there is no longer a risk for infection at these clinics.
Share information about this outbreak and reach out to any friends or family members that may have had procedures at River Side Surgical Center or Clinica K-3 from January 1 to May 13, 2023.
What to Expect
- Healthcare providers will order an MRI scan of your head to look for evidence of infection or complications of meningitis.
- Healthcare providers will perform a spinal tap by inserting a needle into your lower back in a space around your spine to collect fluid for laboratory testing. This is recommended even if you do not currently have symptoms.
- The fluid will be tested in a laboratory to determine if you have fungal meningitis
- If you test positive for infection: your healthcare team will treat you with antifungal medicines. It is possible that you will need to take antifungal medicine for several months to completely cure the infection.
- If you test negative for infection: continue to watch for symptoms for at least 4 weeks from the spinal tap.
- It is possible to test negative at first but still develop meningitis later. Return to the emergency room as soon as possible if you develop new or worsening symptoms.
- If you remain without symptoms, some clinicians may recommend repeating the spinal tap around 2 weeks after your first spinal tap to ensure that you have not developed an infection.
Information for Healthcare Providers
- Healthcare providers should immediately report suspected fungal meningitis cases, including those possibly related to this outbreak, to their state or local health department. Find contact information for your jurisdictional HAI program coordinator.
- See the full Interim Recommendations for diagnosis and management of cases (with or without symptoms) of possible fungal meningitis associated with epidural anesthesia administered in Matamoros, Mexico.The Interim Recommendations document:
- Provides detailed diagnostic and management recommendations for clinicians caring for patients who underwent a procedure under epidural anesthesia in the city of Matamoros.
- Is based on the clinical experience and expert opinion of clinicians caring for patients during the current outbreak or during previous outbreaks of healthcare-associated fungal meningitis in Durango, Mexico, and the United States. It will be updated as additional information becomes available.
- This assessment includes an MRI and lumbar puncture collecting cerebrospinal fluid (CSF) for diagnostic laboratory testing.
Testing Asymptomatic Patients
- Performing the diagnostic assessments in the interim recommendations on all patients with potential exposure, regardless of symptoms, will provide the best chance of preventing widespread morbidity and mortality from this outbreak for the following reasons:
- The latency of symptom onset in some affected patients provides a window of opportunity to identify infection and begin treatment early enough to prevent severe or life-threatening illness:
- Patients without symptoms or with mild symptoms have tested positive for infection.
- Symptom onset ranges from 3 days to 4 weeks after the date of exposure among reported cases to date.
- Fungal meningitis may progress rapidly once symptoms start, causing more severe and harder to treat illness.
- The potential of high case-fatality rates related to this illness:
- A U.S. laboratory and the Mexican national laboratory (InDRE) have reported the detection of the fungusFusarium solanispeciescomplexfrom the CSF (cerebrospinal fluid) of affected patients receiving care in Mexico or the United States. A >40% case-fatality rate was seen in a recent outbreak of central nervous system Fusarium infections in Durango, Mexico (data not published).
Information for Health Departments
Notified Health Departments
- CDC has notified states and local jurisdictions where any patients live who were listed by the Mexican Ministry of Health as potentially at risk.
- Health departments are notifying patients and telling them to seek care (or be evaluated).
- CDC developed resources to assist with patient notification.
- Health departments can email CDC at FungalOutbreak@cdc.gov for resources and additional support.
All Health Departments
- Health departments are encouraged to raise awareness among healthcare providers and the general public in their jurisdictions.
- Additional people with potential exposure who were missing from the original list are being found and contacted through public health investigation, outreach efforts, social media, and by family and friends as they learn about the outbreak.
- For more information about medical tourism and risk mitigation, see CDC Yellow Book 2024: Medical Tourism or contact medicaltourism@cdc.gov.
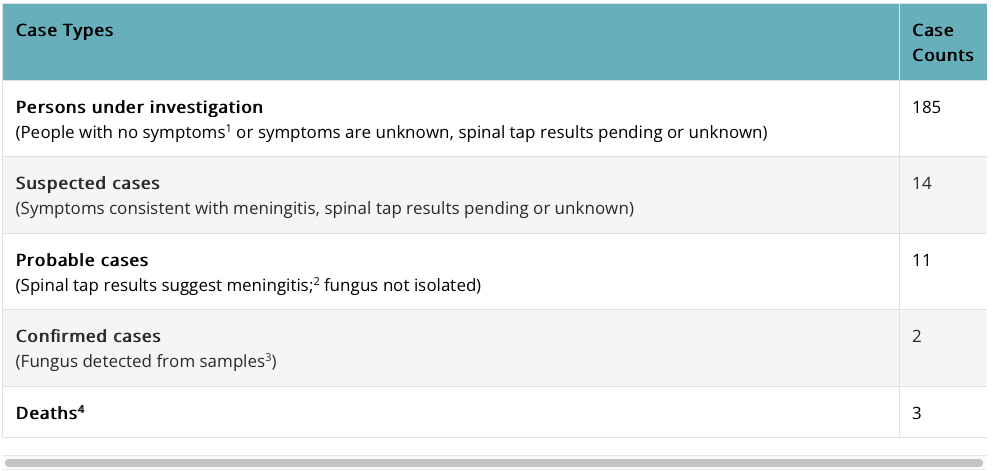
1 Meningitis symptoms include fever, headache, stiff neck, nausea, vomiting, photophobia, and altered mental status.
2 Cerebrospinal fluid (CSF) profile with >5 WBCs/mm3, accounting for the presence of red cells (i.e., subtracting 1 white cell for every 500 RBCs present).
3 Fungus could be detected by culture, polymerase chain reaction (PCR) testing, or metagenomic next generation sequencing (mNGS) testing of CSF or tissue.
4 Two probable cases and one confirmed case.
Findings and Investigations
Select key findings:
- Three U.S. laboratories (CDC Mycotic Diseases Branch’s lab, UCSF Clinical Microbiology Laboratory, and UW Medicine Molecular Microbiology laboratory) and the Mexican national laboratory (InDRE) have detected fungal signals consistent with the Fusarium solanispecies complex from the CSF of patients receiving care in Mexico or the United States.
- Elevated levels of Beta-d-glucan, a biomarker of fungal infection, have been detected in the CSF of some U.S. patients.
Continuing investigations:
- CDC and partners are investigating to determine how people were exposed to the infectious organism(s) during the procedures.
- Officials are investigating whether any additional clinics were involved.
What CDC Is Doing
- Published a Travel Health Notice
- Distributed a Health Alert Notice (HAN) Health Advisory on May 17, 2023
- Published HAN Health Advisory Update
- Collaborated with the Mycoses Study Group to develop Interim Recommendations
- Collaborated with the Mycoses Study Group to produce a webinar discussing epidemiology, diagnostics, and treatment
- Facilitating outreach to potentially impacted patients
- Coordinating and performing specimen testing
- Continuing to investigate the source of the outbreak with colleagues in Mexico
- Disseminating information and strategic outreach to clinicians, the public, and partners
- Providing technical, diagnostic, and clinical advice as requested
Information Source: CDC









