Mega Doctor News
Nat’l ACO Congress VI Features the Physicians’ Role in Patient Engagement
By Roberto Hugo González
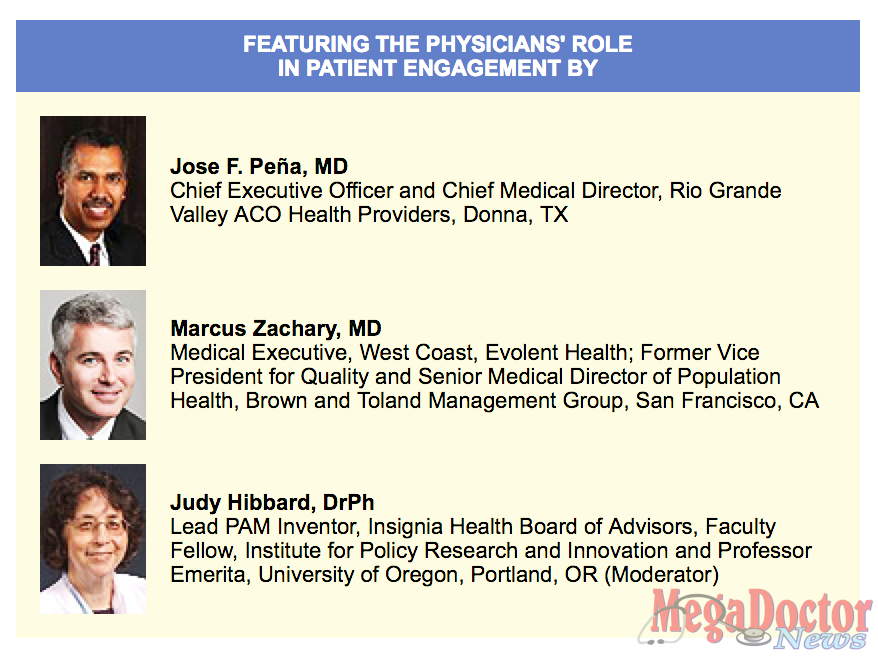
Dr. Jose F. Peña Chief Executive Officer of Donna Medical Group and and Chief Medical Director, Rio Grande Valley ACO Health Providers in Donna, Texas is being featured at The Sixth National Accountable Care Congress taking place in from November 16-18 2015 in Los Angeles California.
Accountable care in both the public and private sector have continued to grow over the past several years, ushering in more experience and evidence on what is working and ways to continue evolving accountable care models.
The Sixth National Accountable Care Congress (www.ACOCongress.com), in Los Angeles, will provide an unprecedented opportunity to discuss remaining barriers to widespread accountable care implementation, strategies to overcome them, and policies to encourage the continued growth and sustainability of the accountable care movement.
The Congress brings together leading policymakers, experts, and accountable care implementers to provide unique and in-depth insights on accountable care implementation and ongoing health care reform.
The Congress will cover a variety of topics including strategies for risk contracting, innovative contract and payment arrangements, physician and patient engagement, state innovations in accountable care, health IT and mobile technology use, opportunities for specialty care and post-acute care integration, employer-led accountable care arrangements, and innovations in contracting for pharmaceuticals and devices. The Congress will also be a great opportunity to explore the future of accountable care contracting, practice, and policies as more organizations are driven to transition to alternative payment models.
WHAT IS AN ACO?
Accountable Care Organizations (ACOs) are groups of physicians, hospitals, and other providers that receive financial rewards for achieving patient-focused quality targets and demonstrating reductions in overall spending growth for their defined patient population. ACOs can be organized in a number of ways, ranging from fully integrated delivery systems to networked models within which physicians in small office practices can work together to improve quality, coordinate care, and reduce costs. ACOs can also feature different payment incentives, ranging from “one-sided” shared savings within a fee-for-service environment to a range of capitation arrangements with quality bonuses. In addition, ACOs are compatible with a range of other payment reforms, such as medical homes and bundled payments; they can help assure that these reforms lead to sustainable quality improvements and cost reductions. In sum, ACOs provide an ideal mechanism to transition from paying for volume and intensity to paying for value.








