Mega Doctor News
By Karen Villarreal
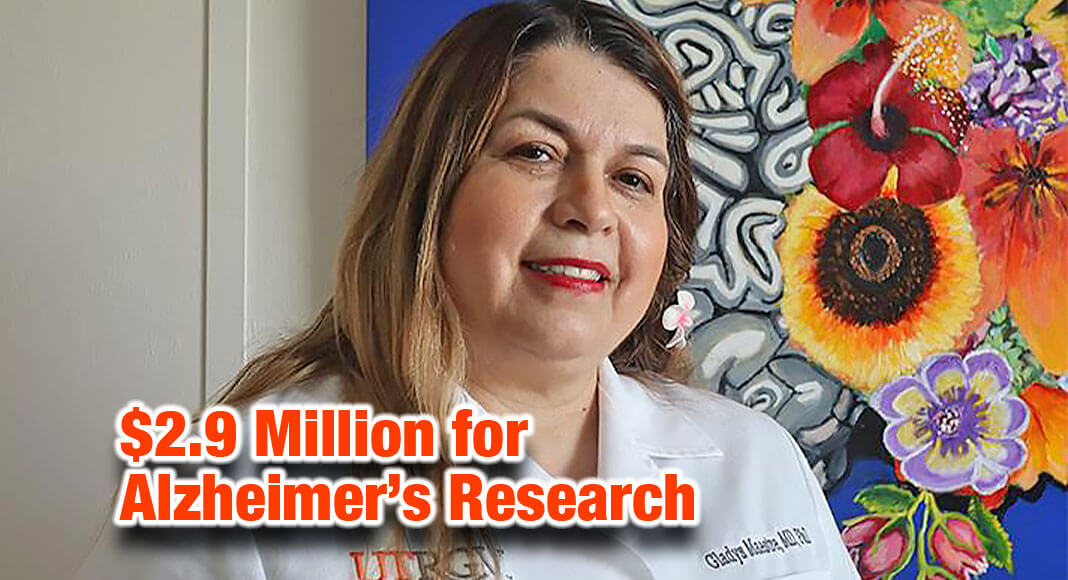
RIO GRANDE VALLEY, Texas – In deep South Texas, where two counties have the highest rate of Alzheimer’s Disease in the country, Dr. Gladys Maestre’s research on the brain is motivated by the Hispanic population’s focus on its elders – and their memory loss.
“Elders are the keepers of the family memories, the efforts of those who tried to improve the family’s situation,” said Maestre, director of the UTRGV School of Medicine’s Alzheimer’s Disease Resource Center for Minority Aging Research.
“Transmitting that part of your history to your children is not going to be through genealogy software even though their popularity shows how many people are looking for that identity.”
Maestre’s previous research found that the rate of memory loss among seniors in parts of South Texas is the highest in the United States – with 20 to 25 percent of seniors in Starr and Zapata counties experiencing Alzheimer’s Disease and related dementias.
That rate is a marked increase from 2016, when 18.9 percent of those on Medicare in Starr County were receiving services to treat Alzheimer’s.
“Let me tell you, I think it’s actually even higher,” said Maestre, who came to UTRGV in 2016 from Columbia University in New York to developa program for better aging. “There are people who are not part of the healthcare system.”
- Texas ranks fourth in the country in the number of Alzheimer’s Disease cases, and second in the number of Alzheimer’s-related deaths.
- The number of Alzheimer’s Disease cases in Texas are expected to increase by 22 percent between 2020 and 2025, from 400,000 to 490,000.
Funded by a $2.9 million grant from the National Institute on Aging, Maestre plans to go door-to-door, starting in Brownsville, to identify more than 2,500 seniors with Alzheimer’s and invite them to participate in the study.
And free testing will be carried out by specialists like UTRGV’s Dr. Frank Gilliam, a neurologist at the university’s Institute of Neuroscience (ION).
MULTI-FACTOR STUDY
Maestre said the study will gather biological data using special technology at the ION facility – MRI scanning; memory tests that utilize virtual reality; eye tracking to investigate facial recognition; and experimental measures like transcranial stimulation, a non-invasive brain stimulation technique known to work for depression and anxiety.
“I’m eager to see if we can use it to improve memory,” Maestre said of transcranial stimulation.
She also plans to look into the impact of addictions on the brain, and bilingualism’s seemingly protective effect against Alzheimer’s, and will conduct physical exams and sleep studies to investigate nocturnal hypertension related to the Alzheimer’s.
The project – “Integration of Socio-Spatial Data for Neighborhoods with Multiomic profiles to Identify and Mitigate Factors Affecting Risk of Alzheimer’s Disease” – additionally investigates social, environmental and economic impacts.
Maestre is particularly interested in Alzheimer’s Disease among Hispanics in underserved communities in the Valley, and she hypothesizes that population is increasingly susceptible to memory loss due to stress and other risk factors. Those factors include poverty, stigma, fear due to citizenship status, and lack of access to public and natural places that encourage physical activity.
- Hispanics in counties with the lowest rate of Alzheimer’s Disease had a greater rate of access to exercise opportunities, with three out of four residents able to readily use those spaces.
- Those opportunities were only available to about half of the residents in counties with the highest rates, like Starr and Zapata.
LONGEVITY VS. QUALITY OF LIFE
Maestre also is investigating positive factors, like family involvement, that seem to play a role in the longer life span of many Hispanics who have Alzheimer’s.
She theorizes that “the Hispanic paradox” – in which a population with less financial resources outlives other racial groups – may be related to the emphasis on family that is so predominant among Hispanics.
- The Hispanic population 65 and older in the United States is projected to grow from 4.6 million in 2019 to 19.9 million by 2060.
- Americans 85 and older, a demographic that likely will require care for memory loss, are expected to increase in number from 509,096 to 3.4 million in 40 years.
- In 2020, there were an estimated 11 million unpaid caregivers in the United States, most of them family members.
“Family comes first here,” she said of Hispanics in South Texas. “Familism is a protective factor for the person with Alzheimer’s, and some people find meaning in caring for their loved ones – the opportunity to spend the last years healing with their family.”
However, while people with early- to middle-stage memory loss often seem happier than before because they don’t have to be aware of reality’s pressures, that same longevity can have a negative impact on family caregivers, Maestre said.
The longer life expectancy can be a serious source of stress, a prolonged struggle with losing the identity of the individual they love, as well as losing their own freedom because so much of their time must be dedicated to caring for the individual with memory loss.
- In Texas, roughly 1.08 million unpaid caregivers provided care to those with Alzheimer’s disease in 2020.
- That equates to an estimated 1.76 billion hours of unpaid care, at a cost of about $25.7 billion a year.
Maestre said she has seen people with Alzheimer’s outlive their caregivers, who neglect their own health by not exercising or sleeping enough because they must check on their parent or spouse.
“Adult children might not have time to date, and some don’t get married because they’re taking care of their parents,” Maestre said. “It might be extreme, almost heroic. That’s what I’ve seen in the Valley – people sacrificing everything.”
SEEKING SOLUTIONS
Maestre said that, in addition to using the technology at the ION, the team will be conducting in-home interviews to identify how to improve the situation for seniors with Alzheimer’s Disease and their families – be it through access to gardens and recreational space, social programs, vitamins and nutrition, or factors yet to be discovered.
“We want to hear from people in the Valley about what they perceive their needs are,” Maestre said. “We want to understand what’s going on at home with clinical symptoms, like irritability, and find the best way to talk about Alzheimer’s Disease to empower the people who look for our help.”
Those interested in participating in the study can email memory@utrgv.edu.
“Participants can remain relatively anonymous,” she said. “We’re just interested in supporting them.”








