
Mega Doctor News
by Mount Sinai Health System
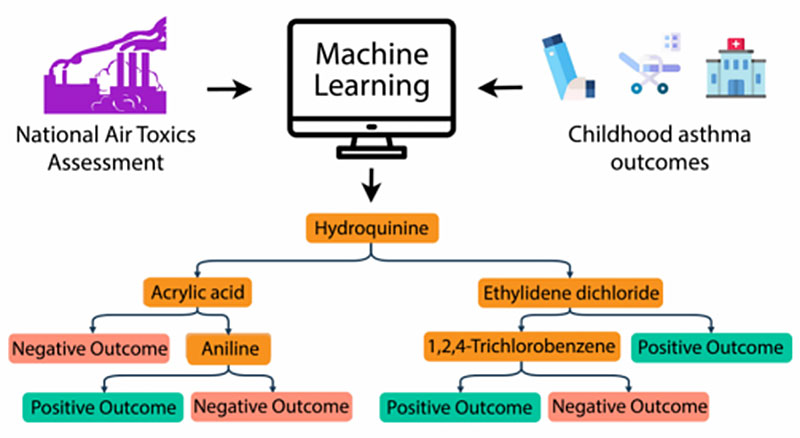
Newswise — Researchers at the Icahn School of Medicine at Mount Sinai have developed a novel machine learning algorithm and used it to identify previously unknown mixtures of toxic air pollutants that appear to be linked to poor asthma outcomes later in a child’s life.
The study examined early exposure to dozens of pollutants potentially experienced by 151 children with mild to severe forms of the disease. While some cases could be linked to an individual, established air pollutant, others appeared to be linked to mixtures of pollutants that had never been associated with asthma. The results and a description of the new algorithm were described in an article in the Journal of Clinical Investigation.
“Asthma is one the most prevalent diseases affecting children in the United States. In this study, we developed a list of air pollutants a young child may be exposed to that can lead to longer-term problems with asthma,” said Supinda Bunyavanich, MD, MPH, MPhil, Professor of Pediatrics, and Genetics and Genomic Sciences, at Icahn Mount Sinai and a senior author of the study. “Our results show how breathing individual and combinations of pollutants may lead to poor asthma outcomes. We hope that having a more comprehensive, holistic view of air pollution may one day be able to reduce the chances that children will be burdened by asthma.”
Affecting about seven percent of children in the United States, asthma is a lung disease that can cause people to wheeze, suffer chest tightness, and bouts of coughing. Although several studies have shown that breathing individual toxic air pollutants, or “air toxics”, raises the chances a child may suffer from asthma, little is known about what happens when the pollutants mix.
In this study, the researchers used a novel machine learning algorithm to find that 18 individual chemicals may be linked to poor asthma outcomes later in life. Specifically, they looked at whether a child needed daily asthma-controlling medication or had to visit an emergency room or spend time in the hospital as a result of their condition. However, they also found new associations between the outcomes and 20 different pollutant mixtures. Several of the chemicals in the mixtures had never been linked to long-term asthma risk.
“Like many scientists, we wanted to provide a more comprehensive picture of how air toxics contribute to childhood asthma,” said Gaurav Pandey, PhD, Assistant Professor of Genetics and Genomic Sciences and a senior author of the study. “Traditionally, for technical reasons, it has been difficult to study the health effects of more than one toxic at a time. We overcame this by tapping into the power of machine learning algorithms.”
The study and development of the algorithm was led by Yan-Chak Li, PhD, a bioinformatician in the Pandey lab, and Hsiao-Hsien Leon Hsu, ScD, Assistant Professor of Environmental Medicine and Public Health at Icahn Mount Sinai.
The researchers first mapped emissions estimates for 125 known pollutants to the residential areas and birth years of 151 children from the New York metropolitan region who were part of Mount Sinai’s Airway in Asthma study. The emissions data were obtained from the Environmental Protection Agency’s National Air Toxics Assessment resource.
Then, the researchers applied a novel algorithm, which they named “Data-driven ExposurE Profile (DEEP) extraction”, to test out whether increased levels of the pollutants observed early in the child’s life were correlated with asthma problems reported around 12 years of age. DEEP relies on a powerful machine learning algorithm called “eXtreme Gradient Boosting (EXBoost), which builds hundreds of “decision trees,” or possible ways that each pollutant, alone or in combination with others, could be associated with the asthma problems seen later in the patient’s lives.
The results showed that some pollutants may have worked alone. For instance, exposure to the ammonia-scented waterproofing agent trimethylamine raised the chances that a child with asthma would have to spend a night in the hospital.
Other pollutants could act alone or in mixtures. Most notably, exposure to acrylic acid raised the chances a child needed daily medication. Mixing acrylic acid with other chemicals not only increased this possibility, but also raised the chances of emergency room visits and overnight hospitalizations.
Interestingly, the researchers also found that some pollutants, such as toluene and cobalt compounds, were only associated with poor outcomes when mixed with other compounds. In fact, 16 of the chemicals they evaluated fell into this category.
“As a physician who treats children with asthma, I was struck by how many potential air toxics are not on our radar,” said Dr. Bunyavanich. “These results changed my view of the heightened risk some children face.”
Finally, the researchers found that demographic factors may play additional roles. For example, exposure to a combination of hydroquinone and ethylidene dichloride was the strongest predictor of overnight hospitalizations. The study found that children who fell into this category were also younger and from lower family incomes than ones who were not exposed to the pollutants.
“Our study is an example of how machine learning has the potential to alter medical research,” said Dr. Pandey. “It is allowing us to understand how a wide variety of environmental factors—or the exposome—influences our health. In the future, we plan to use DEEP and other computer science techniques to tackle environmental factors associated with other complex disorders.”









