Mega Doctor News
By Cynthia Weiss / Mayo Clinic
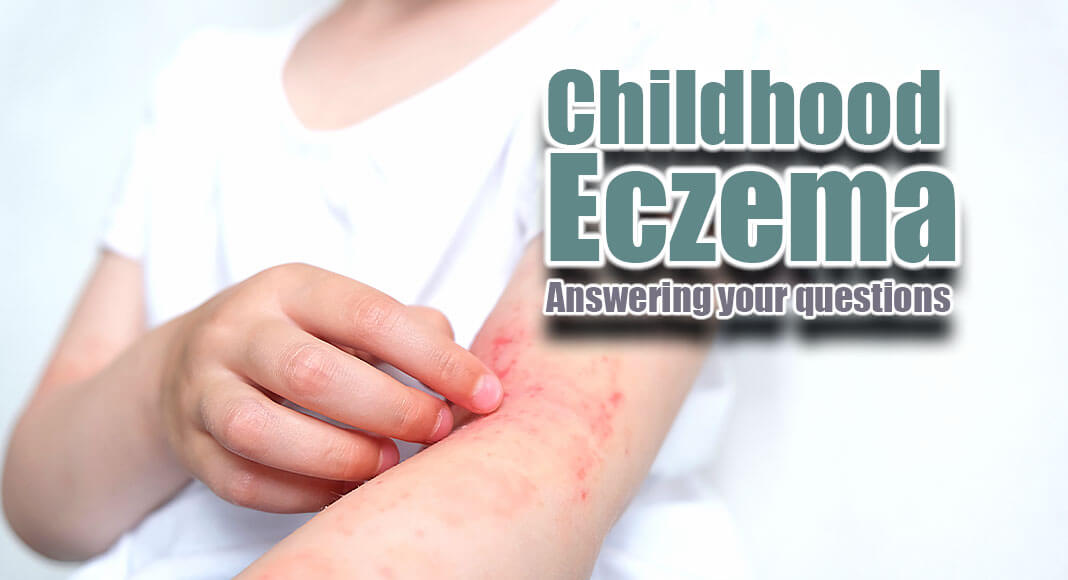
DEAR MAYO CLINIC: My 2-year-old son has a new rash on his arms and back. His doctor said it looks like eczema. He is itching nonstop and that creates red, raw skin. It seems to be worse while he’s lying in bed. No one in the house is getting good sleep because he’s so uncomfortable. What can I do to help him feel better and get some rest?
ANSWER: Itchy and uncomfortable skin is bothersome for adults, but it can be especially difficult for young children. As you have discovered, it can interrupt sleep for the entire family and be a distraction during the day, or cause pain and embarrassment.
Eczema, also called atopic dermatitis, is a common, itchy skin condition in childhood. Most cases begin before age 5, but eczema can occur at any age. It is long-lasting and can appear anywhere on the body.
When a child has eczema, the skin becomes dry and cracked. It can be especially itchy and look like small, raised bumps on the skin. Sometimes, the skin can thicken or darken. It can even become painful when the skin gets raw from intense scratching. Importantly for family and friends, eczema is not contagious.
At its core, eczema is a barrier problem of the skin. Under normal circumstances, the skin acts as a barrier for things moving in and out of the body. When a person has eczema, the barrier is not working as effectively. This allows environmental contaminants to penetrate the skin and protective moisture to leave.
Many things can trigger eczema. Common culprits are fragrances and dyes in products, like laundry detergents, soaps and lotions. Keeping a journal of potential triggers and the child’s skin reaction can be helpful. This doesn’t need to be elaborate, but having a way of documenting symptoms can help to identify eczema triggers for your child.
People with eczema may have other conditions in the “atopic triad,” namely asthma and allergic rhinitis, also called seasonal allergies. Some children have one or two of these conditions, while their siblings have other ones. Researchers are still trying to understand the link between these conditions, but there clearly is a genetic component. Watch for symptoms of asthma and allergic rhinitis as your son grows.
Treating eczema
The best way to treat eczema is to avoid triggers that cause a flare. I recommend that your entire family switches to fragrance-free, dye-free products. Children like to hug and snuggle with parents and siblings, so their clothing and bedding should be fragrance- and dye-free as well to prevent eczema flares.
Medical treatment of eczema begins by controlling skin inflammation. If we can treat skin inflammation, we can control the itch. In the past, eczema often was treated with antihistamines, partly because of the sleepiness they could induce. These medications are used less now because the itch in atopic dermatitis does not appear to be histamine-based.
Usually, the first line of medical treatment is topical steroids. They are effective and time-tested. I often recommend treating eczema using a method called “wet wraps” consistently for two weeks. This is cumbersome but very effective, and it remains a tool for use in the future for subsequent flares. Taking photos before and after treatment is reassuring because improvement in the skin may be subtle at first.
There are lifestyle changes that your family can do at home to reduce eczema flares, such as:
- Apply cream or ointment on the skin at least twice a day to seal in moisture. These products should be specifically formulated for sensitive skin. Generally, lotions are not very effective in atopic dermatitis because they can promote additional water loss.
- Take a short, daily bath or shower using warm — not hot — water. The frequency of bathing is not as important as following the bath or shower with a liberal application of a moisturizer.
- Use gentle cleansers free of dyes, alcohols and fragrances.
- Pat the skin dry after bathing and avoid rubbing. Apply the moisturizer to the slightly damp skin to help “seal in” the moisture.
Most kids will outgrow the constant need to have topical steroids, but the condition is genetically determined, so your son will need to maintain diligence as he gets older. Avoiding products with perfumes and dyes will be a lifelong commitment. — Dr. Kevin Boyd, Dermatology, Mayo Clinic Health System in Onalaska, Wisconsin
Information Source: The Mayo Clinic