Mega Doctor News
The Texas Tribune
When Terry Scoggin left work at Titus Regional Medical Center in Mount Pleasant on Tuesday evening, there were five patients at the facility being treated for COVID.
Overnight, six more people suffering severe coronavirus infections were admitted to the rural Northeast Texas hospital — pushing the facility to its capacity limit and putting Scoggin, the hospital’s chief executive, on high alert for what he’s calling “a fourth surge.”
“We’re at it again,” Scoggin said.
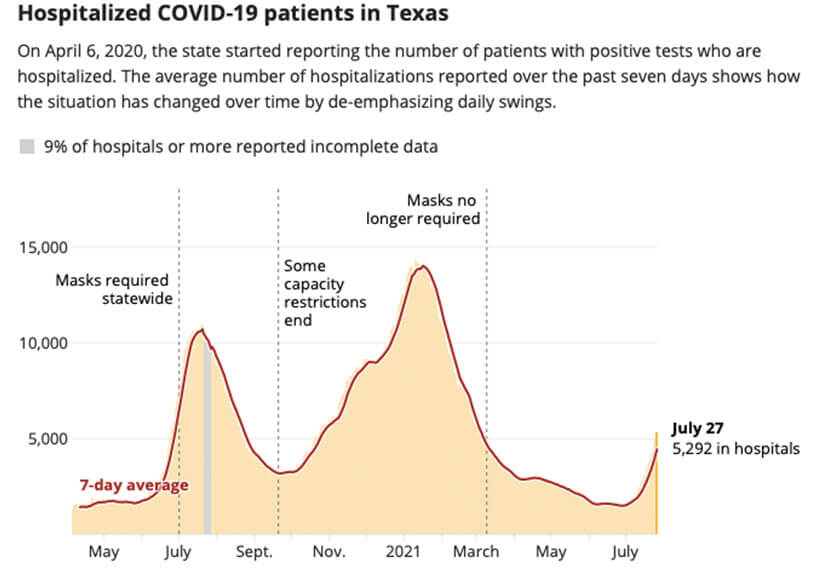
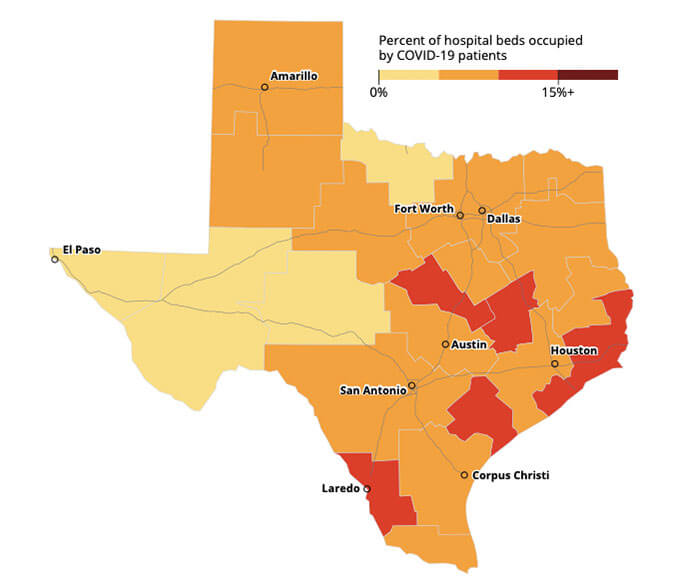
Hospitalized COVID-19 patients in Texas by region
The percentage of hospital beds being used by COVID-19 patients in each trauma service regionshows how the virus is currently impacting hospitals in different parts of the state.
That same night, hospitalizations in Bexar County rose by nearly 8%. Almost 100 people were admitted with severe COVID to local facilities on Tuesday alone, Bexar County officials said on Wednesday.
“These numbers are staggering and frightening,” said Eric Epley, CEO of the Southwest Texas Regional Advisory Council for Trauma in San Antonio.
Hospital and health officials across Texas are seeing similar dramatic jumps, straining an already decimated health care system that is starving for workers in the aftermath of previous coronavirus surges.
In Travis and surrounding counties on Thursday, 314 patients were reported in area hospitals with COVID-19, a number not seen since late February.
In Dallas County, COVID hospitalizations have increased by 99% over the past two weeks, reaching 376 earlier this week. The local numbers are expected to hit between 800 and 1,000 by mid-August, according to forecasters at UT-Southwestern Medical Center.
Overall on Wednesday, Texas hospitals reported 5,292 patients hospitalized with COVID. A week earlier, COVID hospitalizations were 3,566. On July 1, it was 1,591.
“I don’t think we can say it in strong enough terms, what a dangerous situation we’re in right now,” Bexar County Judge Nelson W. Wolff said during a Wednesday news conference.
Fueled by the highly contagious delta variant of the coronavirus, which is contributing to skyrocketing cases not just in Texas but across the nation, the rising hospitalizations rates have spread outside of the heavily populated metro areas that first began to report increases a few weeks ago. Now they are being seen in all corners of the state, triggering pleas from hospitals for state-backed staffing help to handle the increasing pressure.
Trend forecasters at the University of Texas at Austin’s COVID-19 Modeling Consortium said Wednesday that most regions of the state could see a return within a couple of weeks to the capacity-busting hospitalization rate facilities were experiencing in January — the height of the pandemic — if people don’t resume masking up and social distancing.
In Florida, hospitals are already seeing the numbers of COVID patients exceeding levels they saw during the worst of the pandemic, and consortium researchers told The Texas Tribune that Texas is not far behind.
“We are absolutely on a path to hit a surge as large, if not bigger, than the previous surges right now” said Spencer Fox, associate director at the consortium. “If nothing is done, we’re on a crash course for a very large third wave.”
The situation has caused health officials from both rural and metro areas to plead for more resources from the state.
“On behalf of the 157 rural hospitals across Texas, I am writing to ask you immediately take steps to provide additional medical staffing which we anticipate will be needed in our rural hospitals in short order because of the new COVID surge,” John Henderson, president and CEO of the Texas Organization of Rural and Community Hospitals, wrote in a July 26 letter to Gov. Greg Abbott.
Abbott’s office did not immediately respond to requests for comment early Thursday.
In Mount Pleasant, the COVID unit at Titus could typically handle 21 patients — but the facility now only has the nursing staff to cover 6 of those beds, Scoggin said. Transferring new patients to a nearby facility is out of the question, he said. Those who can’t fit in the COVID unit are in the ICU, or the emergency department, or isolated in the labor-and-delivery unit, but that’s not a long-term solution, he said.
“I don’t see another hospital within another 100 miles in a better situation,” Scoggin said.
Henderson said the spoke with a chief nursing officer north of Waco who said that her staff is near collapse after a physically and emotionally exhausting 16 months of fighting the pandemic.
That region, which includes Hill and McLennan counties, has seen one of the sharpest increases in COVID hospitalization rates in the state, according to state health numbers. On July 1, nearly 2% of hospitalizations in the region were COVID patients. By July 27, that had climbed to nearly 10%. Hill County ranks in the bottom half of the state for vaccinated residents.
In the Temple/Killeen region nearby, about 3% of hospitalizations in the area were COVID patients on July 1. By July 27, that had jumped to nearly 14%. In Bell County, only 28% of its residents are fully vaccinated, and it ranks in the bottom third of all 254 counties in residents who’ve gotten at least one vaccine shot.
“Not all of [the] nursing staff is fully vaccinated, but the ones who are literally are in tears, knowing that they’re about to go through, again, what they’ve been through before, and how terrible it’s going to be,” Henderson said.
The push to vaccinate
Upwards of 95% of those who are being hospitalized are unvaccinated, officials in Bexar, Travis and other counties say.
“Nearly every COVID patient admission is completely preventable,” said Dr. Bryan Alsip, executive vice president and chief medical officer at University Health System in San Antonio. “Staff witness this every day and it’s very, very frustrating.”
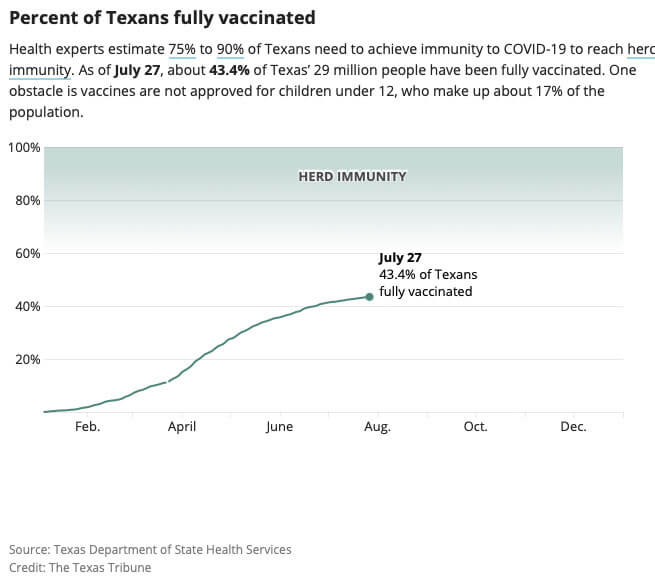
Vaccination rates have been increasing in recent days, but some 16 million Texans are still not fully vaccinated. That’s more than half of the state population, including children under 12 who are still too young to get the injection.
On Tuesday, the U.S. Centers for Disease Control and Prevention sounded the alarm about the rising cases and rates, urging masks for vaccinated people in substantial- and high-transmission areas — which includes almost all of Texas’ 254 counties — and for everyone in schools, regardless of vaccination status or region.
The reason for the CDC’s reversal on masks for the vaccinated, which agency officials said in May were no longer necessary, is that emerging science indicates that the delta variant is more transmissible through what they called “rare breakthrough infections” of vaccinated people than the earlier versions of the virus.
Those infections don’t cause hospitalizations in most cases but can still contribute to community spread and endanger those who are not protected by the vaccine, CDC officials said. The best protection against that, in the short term, is masking and social distancing to flatten the curve, health officials say.
But so far, Republican state leaders have declined to reinstate stay-at-home orders, mask mandates, vaccine mandates, or other pandemic-era protocols, and continue to ban local governments from creating their own.
Instead, Abbott and Texas State Health Commissioner Dr. John Hellerstedt have increased their push for more people to get vaccinated.
But UT forecasters, whose modeling programs forecasting surges last summer gained national attention, say new vaccinations won’t stop the surge that could hit the state in the first two weeks of August.
According to the UT models, without any behavioral changes like masking and other safety practices, Texas could reach more than 14,000 COVID hospitalizations by Aug. 12 — the same number Texas saw at the height of the surge in mid-January, and just as millions of Texas students start returning to school.
“Vaccination is our endgame, our long-term solution to all of this to protect our communities,” Fox said. “But right now, in the midst of a surge, it’s not going to prevent the strain on health care capacity. What we need is behavioral change, like what we saw during the summer wave and the winter wave.”
Staving off the surge
In the absence of mandates or statewide protocols, and as the state gets more aggressive in its efforts to vaccinate people with increasing public awareness campaigns and more pop-up vaccine clinics, local health and government officials are desperately looking for ways to slow infections or keep the newly infected healthy enough to stay out of the hospital.
In Mount Pleasant, Scoggin credits monoclonal antibody treatments — two-hour infusions of the drug Regeneron done on an outpatient basis that lower the severity of the virus if treatments are started early enough — with keeping his numbers barely manageable so far. His facility is giving the treatments to at least five patients per day now, he said.
“We didn’t give that many at any point during our other surges, so we were admitting them before — but this time there are more who are outpatients,” Scoggin said. “That’s a good thing, because we couldn’t handle any more than we have in the hospital right now.”
Bexar County officials said on Wednesday that a regional infusion center would be opening within the next week to keep people out of hospitals. During the last surge, Wolff said, an area infusion center treated up to 90 people a day and was “a great success.”
The county, along with other metro areas, is also asking the state for permission to mandate masks for governmental employees and in schools, officials said.
Last Friday, Austin went to Stage 4 in its risk-based guidelines for the first time since the winter, prompting some summer day camps to close and other businesses to reinstate masking requirements for customers.
Austin Mayor Steve Adler, wearing a mask during this week’s City Council meeting, said he hoped the city could find a way to require its employees to be vaccinated in spite of Abbott’s ban on vaccine mandates.
Henderson, head of the rural hospital organization, said the worst part of the entire scenario is that it could have been avoided with more acceptance of the vaccine, particularly in rural areas.
“It’s tragic, and it’s avoidable,” he said. “We’re our own worst enemy at this point.”
Chris Essig contributed to this report.
A patient received their first dose of a COVID-19 vaccine at a clinic held in partnership between the Central Texas Food Bank and University of Texas in Austin on July 21, 2021. Credit: Sophie Park/The Texas Tribune