Mega Doctor News
By Jaime Aron, American Heart Association New
There are plenty of reasons why 1 in 5 Americans live in rural areas.
Start with the most basic: It may be where they were born and raised, like their parents and perhaps their parents. Maybe they like their neighbors. Or the pace. Or they enjoy open spaces, especially those framed by some of nature’s most beautiful sights. Heck, maybe it’s just because that’s where life landed them.
Whatever the reason, and wherever the location, far too many of the roughly 66 million people who 2020 census data show live in rural America share a disturbing reality: They lack access to quality health care.
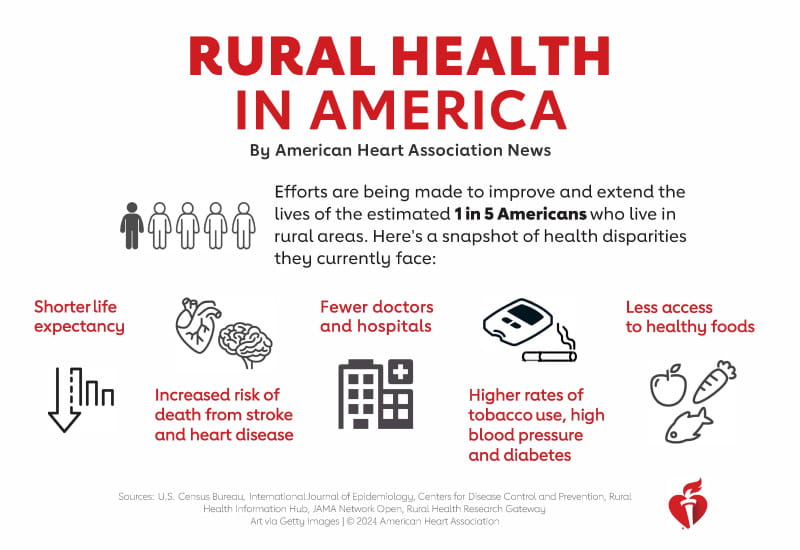
Research conducted before the COVID-19 pandemic shows the life expectancy of rural Americans overall is about 2.5 years less on average than for people in urban settings – and rural residents are more likely to die early from heart disease and stroke.
Shorter life spans and more illnesses are byproducts of accumulated risk factors that also stack up more for rural folks compared to urban and suburban dwellers. These include higher rates of tobacco use, physical inactivity, obesity, diabetes and high blood pressure.
Why?
At the root, it’s a numbers game. There are fewer doctors and hospitals in rural areas (and those numbers are spiraling down), which means less specialized care.
So, getting care can require covering a lot of miles, which of course can take a lot of time – which, in an emergency, is precious time. And that’s in good weather. The expanse of miles also brings challenges of getting people enough food, much less healthy food.
There’s no single fix, of course. The issues are as complex and varied as the places themselves.
A snapshot of health disparities faced by Americans who live in rural areas. (American Heart Association)
The American Heart Association has long worked with people in rural America to level the playing field. A few years ago, the organization kicked things up a notch.
A “presidential advisory” is a rare step taken to address a topic of special importance. It’s a way of letting everyone know there’s a problem that needs extra attention. The AHA released a presidential advisory titled “Call to Action: Rural Health.” It emphasized the need for increased access to care, improved quality of health care and a more targeted approach to reducing risk factors.
It was released in February 2020. Weeks later, the COVID-19 pandemic arrived. Much like the way the virus exposed system flaws in social issues, rural Americans were disproportionately affected, too. What already was a crisis became even worse.
“My comments from four years ago are just as relevant today as in 2020,” said Dr. Robert Harrington, the dean of Weill Cornell Medicine in New York City who was the AHA president at the time of the advisory. “And, certainly, the pandemic continued to highlight these health disparities, especially as we witnessed hospital closures in rural America.”
In response to many issues exposed by the pandemic, the AHA created a 2024 Impact Goal aimed at improving health equity for all, including identifying and removing barriers to health care access and quality. Health problems in rural America are one of those barriers.
In 2022, the AHA launched a three-year initiative to help rural hospitals and clinicians provide high-quality, consistent, timely and appropriate evidence-based care. The organization also created HeartCorps, which puts service-minded adults into rural communities to improve heart health. Last summer, the AHA announced a $20 million investment into scientific research of health challenges in rural areas.
These moves are in addition to many more ongoing programs, such as expansion of Mission: Lifeline, which has been shown to reduce response time and improve outcomes for patients in need of acute care for heart problems and stroke since 2010. The organization also continues to push for policy changes, such as getting millions more people access to Medicaid and telehealth.
Of course, there are important quality of life areas where rural communities shine.
Start with the emphasis on the word “community.” Even in places where next-door neighbors might be a mile away, folks pitch in for barn raisings and potluck dinners; when major life events occur – happy or sad – folks gather quickly and rare is the person who goes away hungry. In some cases, these powerful bonds generate higher levels of social connectivity and engagement.
This introduction is not a deep dive into the complexities of health in rural America. It’s also not meant to paint a doom-and-gloom portrait; quite the opposite, it’s meant to be a reminder of the importance of improving and extending the lives of this sometimes-overlooked segment of the country.
Ultimately, this single story is merely an overview of health in rural America – the proverbial 10,000-foot view of the landscape.
A better understanding of the challenges and triumphs requires being down on the ground, in the thick of it, talking to the people who call rural America “home.”
So American Heart Association reporters, photographers and videographers visited five largely rural states. Week by week, state by state, we will publish stories about what they found. Accompanying each will be images and videos showcasing the people, the issues and the beauty of these places.
- From North Dakota, a look at how health care professionals are turning to telemedicine and community education to cope with health care challenges.
- From Kansas, a look at the Iowa Tribe of Kansas and Nebraska’s efforts to improve healthy food access and cultivate food sovereignty to help feed residents of their community, which is about a half-hour drive from the nearest grocery store. It’s part of the Ioway’s shift to regenerative agriculture after realizing contaminants in their soil were killing their … bees.
- From West Virginia, a state with some of the highest rates of chronic illness in the nation, a look at how community health workers step in to provide home-based medical support and so much more; and the challenges of breaking a generational cycle of heart disease by slowly shifting families away from culturally entrenched, unhealthy eating patterns, a tale told through the mother-daughter team of Sabrina Ford and Sarah Ward, two health care workers at the only clinic in an Appalachian town of about 1,200 people.
- From Kentucky, a look at navigating hilly, winding, GPS-unfriendly roads that strain the emergency response system; and how state legislation and the efforts of local emergency medical services led to an improved system of care for heart patients.
- And from Alaska, a look at how all the challenges everywhere in rural America are compounded by the extremes of being in such a big, cold, remote state in which half the population is bunched in one spot and the other half is spread across incredibly vast distances, plus the fact there are two health care systems: the standard conglomeration of public and private options for about 80% of residents, and another system for Alaska Native and American Indian people living in Alaska.
Back to the presidential advisory, the AHA writing group stressed three topics to consider: urban-rural disparities in health outcomes, the differences (urban versus rural) in the social determinants of health, and complex health delivery system differences in rural versus urban areas.
“Addressing the unique health needs of people in rural America is critical to the American Heart Association’s mission to create a world of longer, healthier lives,” Harrington said when the advisory was released.
“And,” he said recently, “it’s still true today!”









