Mega Doctor News
Newswise — Researchers at Albert Einstein College of Medicine have designed an experimental drug that reversed key symptoms of Alzheimer’s disease in mice. The drug works by reinvigorating a cellular cleaning mechanism that gets rid of unwanted proteins by digesting and recycling them. The study was published online today in the journal Cell.
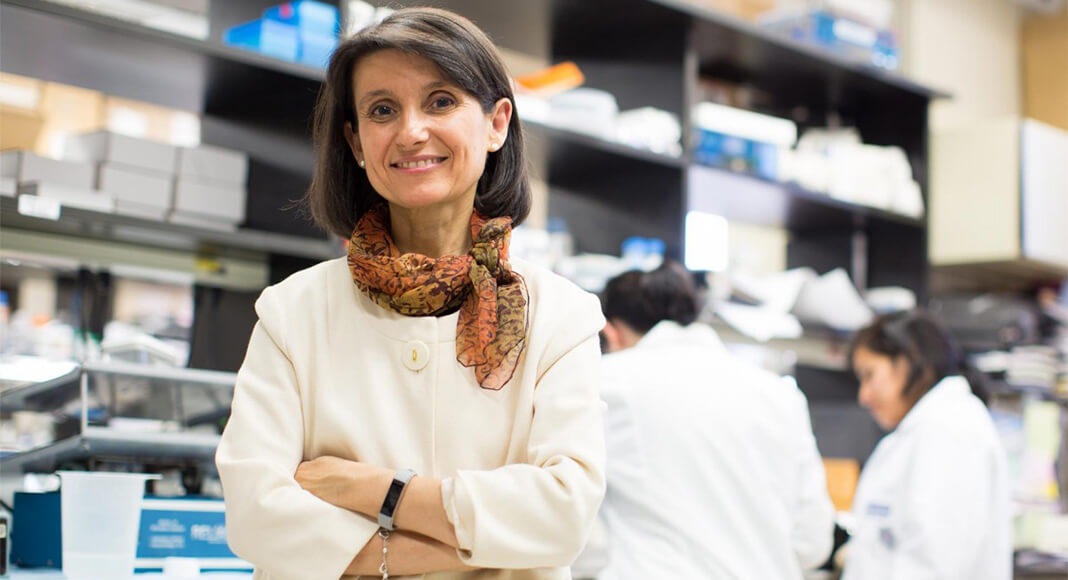
“Discoveries in mice don’t always translate to humans, especially in Alzheimer’s disease,” said co-study leader Ana Maria Cuervo, M.D., Ph.D., the Robert and Renée Belfer Chair for the Study of Neurodegenerative Diseases, professor of developmental and molecular biology, and co-director of the Institute for Aging Research at Einstein. “But we were encouraged to find in our study that the drop-off in cellular cleaning that contributes to Alzheimer’s in mice also occurs in people with the disease, suggesting that our drug may also work in humans.” In the 1990s, Dr. Cuervo discovered the existence of this cell-cleaning process, known as chaperone-mediated autophagy (CMA) and has published 200 papers on its role in health and disease.
CMA becomes less efficient as people age, increasing the risk that unwanted proteins will accumulate into insoluble clumps that damage cells. In fact, Alzheimer’s and all other neurodegenerative diseases are characterized by the presence of toxic protein aggregates in patients’ brains. The Cell paper reveals a dynamic interplay between CMA and Alzheimer’s disease, with loss of CMA in neurons contributing to Alzheimer’s and vice versa. The findings suggest that drugs for revving up CMA may offer hope for treating neurodegenerative diseases.
Establishing CMA’s Link to Alzheimer’s
Dr. Cuervo’s team first looked at whether impaired CMA contributes to Alzheimer’s. To do so, they genetically engineered a mouse to have excitatory brain neurons that lacked CMA. The absence of CMA in one type of brain cell was enough to cause short-term memory loss, impaired walking, and other problems often found in rodent models of Alzheimer’s disease. In addition, the absence of CMA profoundly disrupted proteostasis—the cells’ ability to regulate the proteins they contain. Normally soluble proteins had shifted to being insoluble and at risk for clumping into toxic aggregates.
Dr. Cuervo suspected the converse was also true: that early Alzheimer’s impairs CMA. So she and her colleagues studied a mouse model of early Alzheimer’s in which brain neurons were made to produce defective copies of the protein tau. Evidence indicates that abnormal copies of tau clump together to form neurofibrillary tangles that contribute to Alzheimer’s. The research team focused on CMA activity within neurons of the hippocampus—the brain region crucial for memory and learning. They found that CMA activity in those neurons was significantly reduced compared to control animals.
What about early Alzheimer’s in people—does it block CMA too? To find out, the researchers looked at single-cell RNA-sequencing data from neurons obtained postmortem from the brains of Alzheimer’s patients and from a comparison group of healthy individuals. The sequencing data revealed CMA’s activity level in patients’ brain tissue. Sure enough, CMA activity was somewhat inhibited in people who had been in the early stages of Alzheimer’s, followed by much greater CMA inhibition in the brains of people with advanced Alzheimer’s.
“By the time people reach the age of 70 or 80, CMA activity has usually decreased by about 30% compared to when they were younger,” said Dr. Cuervo. “Most peoples’ brains can compensate for this decline. But if you add neurodegenerative disease to the mix, the effect on the normal protein makeup of brain neurons can be devastating. Our study shows that CMA deficiency interacts synergistically with Alzheimer’s pathology to greatly accelerate disease progression.”
A New Drug Cleans Neurons and Reverses Symptoms
In an encouraging finding, Dr. Cuervo and her team developed a novel drug that shows potential for treating Alzheimer’s. “We know that CMA is capable of digesting defective tau and other proteins,” said Dr. Cuervo. “But the sheer amount of defective protein in Alzheimer’s and other neurodegenerative diseases overwhelms CMA and essentially cripples it. Our drug revitalizes CMA efficiency by boosting levels of a key CMA component.”
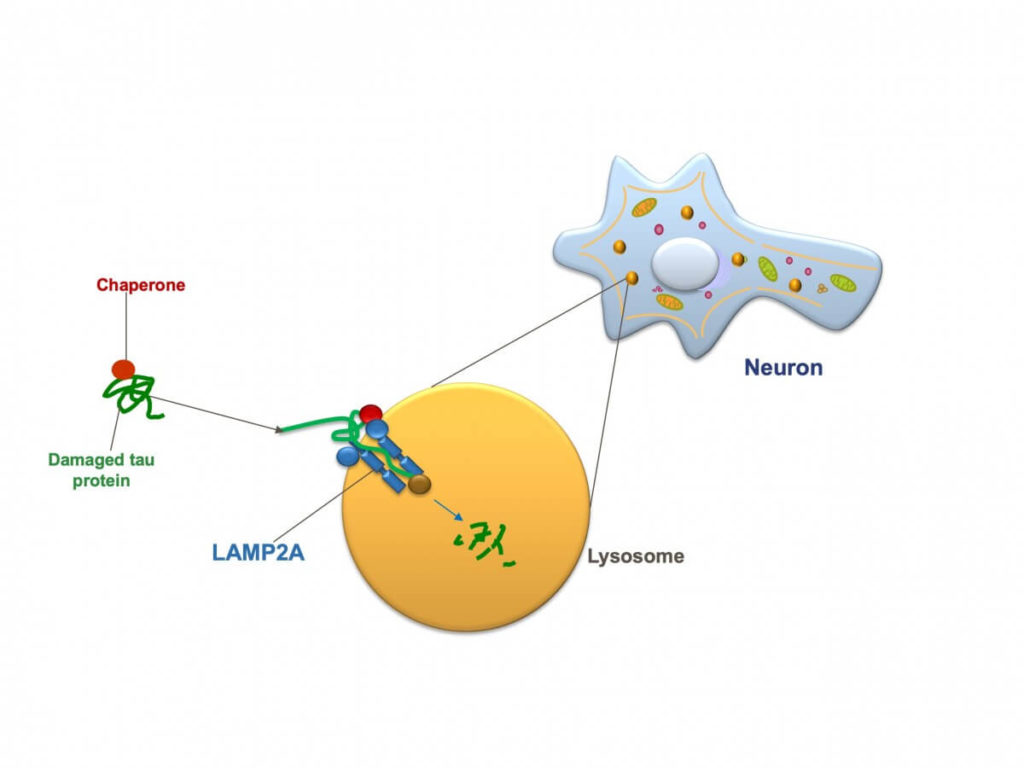
In CMA, proteins called chaperones bind to damaged or defective proteins in cells of the body. The chaperones ferry their cargo to the cells’ lysosomes—membrane-bound organelles filled with enzymes, which digest and recycle waste material. To successfully get their cargo into lysosomes, however, chaperones must first “dock” the material onto a protein receptor called LAMP2A that sprouts from the membranes of lysosomes. The more LAMP2A receptors on lysosomes, the greater the level of CMA activity possible. The new drug, called CA, works by increasing the number of those LAMP2A receptors.
“You produce the same amount of LAMP2A receptors throughout life,” said Dr. Cuervo. “But those receptors deteriorate more quickly as you age, so older people tend to have less of them available for delivering unwanted proteins into lysosomes. CA restores LAMP2A to youthful levels, enabling CMA to get rid of tau and other defective proteins so they can’t form those toxic protein clumps.” (Also this month, Dr. Cuervo’s team reported in Nature Communications that, for the first time, they had isolated lysosomes from the brains of Alzheimer’s disease patients and observed that reduction in the number of LAMP2A receptors causes loss of CMA in humans, just as it does in animal models of Alzheimer’s.)
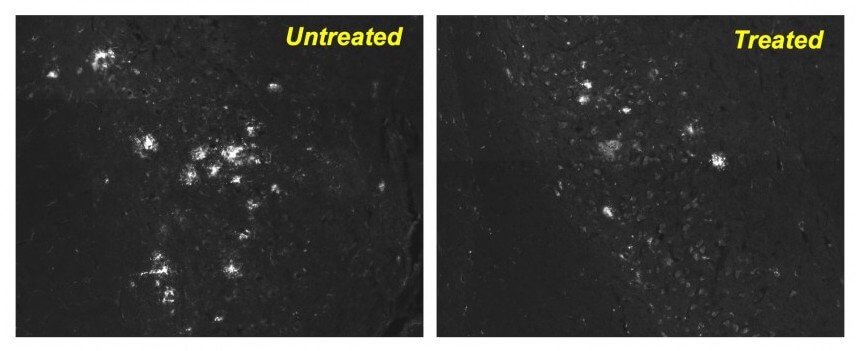
The researchers tested CA in two different mouse models of Alzheimer’s disease. In both disease mouse models, oral doses of CA administered over 4 to 6 months led to improvements in memory, depression, and anxiety that made the treated animals resemble or closely resemble healthy, control mice. Walking ability significantly improved in the animal model in which it was a problem. And in brain neurons of both animal models, the drug significantly reduced levels of tau protein and protein clumps compared with untreated animals.
“Importantly, animals in both models were already showing symptoms of disease, and their neurons were clogged with toxic proteins before the drugs were administered,” said Dr. Cuervo. “This means that the drug may help preserve neuron function even in the later stages of disease. We were also very excited that the drug significantly reduced gliosis—the inflammation and scarring of cells surrounding brain neurons. Gliosis is associated with toxic proteins and is known to play a major role in perpetuating and worsening neurodegenerative diseases.”
Treatment with CA did not appear to harm other organs even when given daily for extended periods of time. The drug was designed by Evripidis Gavathiotis, Ph.D., professor of biochemistry and of medicineand a co-leader of the study.
Drs. Cuervo and Gavathiotis have teamed up with Life Biosciences of Boston, Mass., to found Selphagy Therapeutics, which is currently developing CA and related compounds for treating Alzheimer’s and other neurodegenerative diseases.
The study is titled, “Chaperone-mediated autophagy prevents collapse of the neuronal metastable proteome.” The study’s other co-leader and first author is Mathieu Bourdenx, Ph.D., a postdoctoral fellow in Dr. Cuervo’s lab and also a junior researcher at the Institute of Neurodegenerative Diseases, University of Bordeaux, France. Additional Einstein authors include: Adrián Martín-Segura, Aurora Scrivo, Susmita Kaushik, Ph.D., Inmaculada Tasset, Ph.D., Antonio Diaz and Yves R. Juste.
Other contributors include: Jose A. Rodriguez-Navarro (formerly at Einstein) at Hospital Universitario Ramón y Cajal, Madrid, Spain, Nadia J. Storm (formerly at Einstein) at University of Copenhagen, Denmark, Qisheng Xin (formerly at Einstein), Erica Stevenson, Nevan Krogan and Danielle L. Swaney both at University of California at San Francisco, CA, Enrique Luengo at Universidad Autonoma de Madrid, Madrid, Spain, Cristina Clement, Ph.D., and Laura Santambrogio, M.D., Ph.D., both at Weill Cornell Medicine, New York, NY, Se Joon Choi, Ph.D., Eugene V. Mosharov and David Sulzer, Ph.D., all at Columbia University Medical Center, New York, NY and Fiona Grueninger, Ph.D., and Ludovic Collin both at Roche Pharma, Switzerland.
The study was supported by the National Institutes of Health (AG054108, AG021904, AG017617, AG038072, AG031782, NS100717, NS095435), the JPB Foundation, the Rainwater Charitable Foundation, Michael J. Fox Foundation, and the Backus Foundation.
Drs. Cuervo and Gavathiotis are cofounders and scientific advisory board members of Selphagy Therapeutics Inc. now part of Life Bioscience (Boston, MA). CA compound is under the following patent: Retinoic acid receptor antagonists as chaperone-mediated autophagy modulators and uses thereof; Gavathiotis E, Cuervo AM, Xin Q, Das BC; United States patent granted US9512092; 2016 Dec 16. The remaining authors declare no competing interests.